
Our network of licensed mental health professionals is ready to help.

Everyone feels down or sad sometimes. But when low feelings are intense, long-lasting or make daily life difficult, it might be depression, a common but serious mood disorder. Learn the causes, symptoms, and treatments now.
We all experience low moods from time to time. But unlike distressing feelings such as sadness or irritation that come and go depending on what’s happening in your life, depression doesn’t lift.
It can last for weeks, months or even years, and it can impact more than just your mood. Depression also affects how you think and function in your daily life. You might feel down a lot of the time — or all of the time — and find it hard to concentrate.
Depression can also cause foggy thinking, and it might even make you talk and walk more slowly. That’s because depression can interfere with the brain’s process of having a thought, such as “walk to the bedroom,” and your ability to follow through on that action.
If you think you have depression, you might feel very alone. But know that you’re not. Depression is one of the most common mental illnesses. In fact, about 16% of Americans will experience depression at some point in their lives, according to the Centers for Disease Control and Prevention.
The good news: There are a number of treatments proven to help ease the symptoms of depression and get you back on track. The key is partnering with the right health care provider and therapist to figure out the best course for you.

Our network of licensed mental health professionals is ready to help.
Depression is a mood disorder that affects your everyday emotions and thinking. Mood disorders are more intense and harder to manage than normal feelings of sadness or guilt, which are temporary.
Depression is different for everyone, but often the earliest signs are feeling down and very negative. Someone might make a comment that you ordinarily wouldn’t take personally, but now it feels very hurtful or upsetting. You may even begin to feel numb and unable to experience joy and pleasure in things you love, such as walking your dog or watching a favorite show.
The exact cause of depression isn’t always known, and there’s usually more than one factor at play. Everything from your genetics to not getting enough sleep can bring on depression.
A major life change, especially a negative one such as the death of someone you love (including a pet), a divorce or job loss can also trigger depression. Changes in your brain chemistry, including from taking certain medications or recreational drugs, can also bring it on. And sometimes it’s not clear what has triggered it.
People from certain backgrounds or those who have certain traits are more likely to experience depression than others. For example, women experience major depressive episodes at a rate of 8.7%, compared to 5.3% for men, according to the National Institute of Mental Health. And non-Hispanic white and non-Hispanic black Americans are the most likely to experience depression of any severity.
While you can have depression at any age, some age groups experience it more often than others, according to the Centers for Disease Control and Prevention:
There isn’t just one category of depression. There are several, and depending on your symptoms or the cause of your symptoms, your health care provider can determine which type you are experiencing.
Major depressive disorder/major depression. Major depression is a serious disorder, during which you feel very depressed most of the time for more than 2 weeks.
A person with major depression finds it difficult to do even the most basic things, including dressing, working and talking with others. It usually occurs in cycles. Symptoms can develop and last for days or weeks and then they may go away for periods of time.
Dysthymia/persistent depressive disorder. Dysthymia is a mild to moderate low mood that lasts daily for more than 2 years. Some people may think they are naturally glass-half-empty types, when in fact they are suffering from dysthymia.
Postpartum depression. This is major depression that occurs after having a baby. Postpartum depression is more intense and lasts longer than the typical “baby blues,” which many women get in the days after giving birth. Baby blues are often due to fluctuating hormones.
While the baby blues usually go away after about 2 weeks, postpartum depression is longer-lasting and more severe. It can even begin up to a year after giving birth.
Symptoms of postpartum depression can include:
In more severe situations, you may even have thoughts of harming yourself or the baby. (This can be incredibly frightening, and if you experience any of these thoughts, reach out to your health care provider as soon as possible.)
Prenatal depression, which happens less often than postpartum depression, is any depression that occurs during pregnancy, according to the National Institute of Mental Health. Talk to your health care provider if you have symptoms of depression while you’re pregnant.
Psychotic depression. Psychotic depression is major depression plus some form of psychosis. People with psychosis have delusions. Or they hear or see upsetting things that aren’t really there (hallucinations).
Seasonal affective disorder (SAD). As the name implies, SAD is seasonal depression that occurs most often during the winter months, when there is less natural sunlight. It’s more severe than the usual “winter blues,” and it sometimes improves with light therapy.
Bipolar disorder. Someone with bipolar mood disorder will experience extremely low moods that meet the criteria for major depression. However, those periods may alternate with periods of mania, which include extreme highs, such as feeling very happy or “wired.”
During a manic period, someone might talk quickly, have a decreased need for sleep, or start grandiose projects but struggle to finish them. During a depressed period, they might feel very tired, sad and hopeless. They may also find it hard to accomplish normal day-to-day tasks, such as working or going to school.
Disruptive mood dysregulation disorder. This disorder is diagnosed in children and adolescents who have severe and regular temper outbursts. These events are more intense and frequent (3 or more times a week for a year or more) than a typical tantrum.
Premenstrual dysphoric disorder (PMDD). This type of depression typically begins the week before menstruation and tapers off a few days after your period starts. Symptoms can include severe mood swings, anxiety and trouble concentrating or sleeping.
This is different from more common premenstrual syndrome (PMS), which may make you feel moody, irritable and weepy. With PMS, you’re still able to carry on with your usual life. PMDD, on the other hand, is much more disruptive.
Your primary care provider (PCP) may be the first medical professional to screen you for depression. So if you’re feeling low, it’s important to speak up. Most doctors ask their patients questions at regular checkups that can clue them in to how the patient is feeling, including questions about mood and behavior.
Your doctor will also be on the lookout for certain risk factors for depression, including:
After the screening, your doctor might want you to visit a mental health professional for an official diagnosis and to figure out a treatment plan. Mental health professionals can include psychiatrists, psychologists and licensed therapists. Some primary care doctors also feel comfortable treating depression themselves.

Your doctor or mental health professional will determine which symptoms you have and how long they’ve lasted. For example, to be diagnosed with major depression, you must have at least 5 of the 9 symptoms listed below. Plus, you must also have at least 1 of the first 2 symptoms nearly daily for at least 2 weeks:
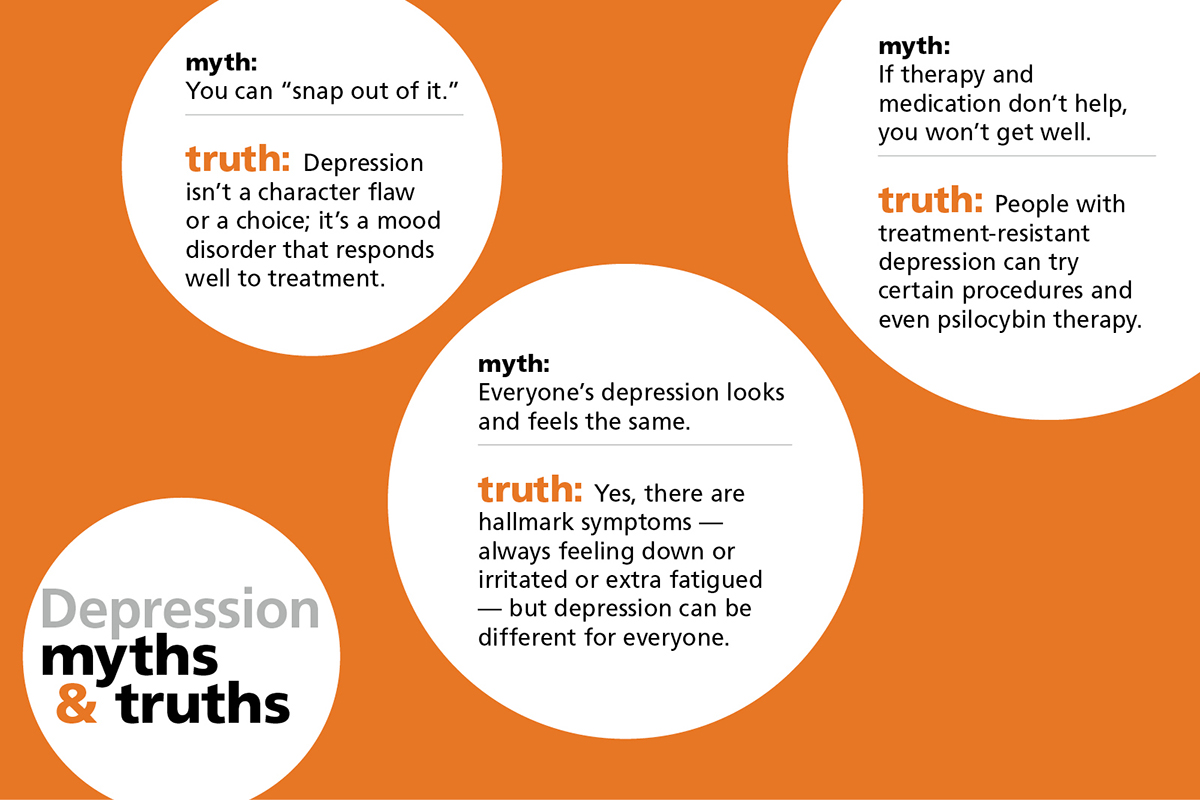
Every person with depression will experience it somewhat differently. Some folks with major depression may also experience anxiety, irritability or guilt. For others, a sense of hopelessness and a lack of purpose can creep in.
People with depression report that it often feels like they lose a sense of themselves and their connection to others, even when they’re around loved ones. Some describe it as a feeling that the spark of life has been dimmed. How severe these symptoms are and how long they last vary from person to person.
Men and women sometimes experience depression differently, too. Men might be more irritable, pessimistic and defensive; they often don’t sleep well and stay up late. Women are more likely to have both a low mood and feelings of hopelessness. And although men die by depression-related suicide more often than women, women are more likely to have suicidal thoughts with depression.
One thing to remember: If you’re experiencing any of these feelings, it’s not your fault. You didn’t do anything to create or cause them. But you can take action to manage them.
There’s no one-size-fits-all fix. But the most common recommendations for treating depression are therapy and medication. Lifestyle changes, such as exercising and socializing more, can help too. Not everyone with depression will need to take medication, but therapy is strongly recommended for anyone suffering from the condition.
A mainstay of depression treatment is psychotherapy, also called talk therapy. A therapist helps you identify and cope with troubling emotions, thoughts and behavior.
Therapy can help you learn strategies to handle stressful situations. Therapy can also teach you how to replace negative beliefs and self-defeating behaviors with healthy alternatives. A therapist can also support you in making positive changes to your relationships and help you set healthy goals. (Find a new therapist now.)
Some therapists specialize in treating depression. They may use one or more approaches to help ease symptoms and improve a person’s thinking and outlook. Here are some common types of therapy that can help:
Cognitive behavioral therapy. This approach focuses on thoughts and beliefs and how they influence your mood and actions. You will learn how to shift long-held thinking patterns by challenging untrue beliefs about yourself and others. You’ll also learn to reassess things in a more hopeful light.
Behavioral activation. When you’re depressed, you may find yourself avoiding challenging situations or isolating yourself. These behaviors can make depression symptoms worse. Behavioral activation teaches you how to counter those tendencies.
Family therapy. Just as the name suggests, family therapy provides professional support to both the person diagnosed with depression and their family members. This can be important: Depression doesn’t just impact the person struggling with it — everyone around them can be affected, too.
Once you have the names of a few therapists, you can set up consultations to see if any of them would be a good fit for you. The first session is often called an intake session. The therapist will gather information from you and decide the best way to proceed. You can also prepare a list of questions to ask the therapist to help you determine whether they’re the right match for you. Here are some starter questions:
It’s important to have a good relationship with your therapist, so listen to your gut. But a helpful therapist should also challenge you. That can feel uncomfortable at first, but it’s totally normal, especially if it’s your first time seeking counseling. And remember that you can switch therapists at any time, if necessary.
Learn more about how to prep for your first visit here.
The other side of depression treatment is antidepressant medication. There are many different types, and most target brain chemicals called neurotransmitters. Those chemicals, such as serotonin, norepinephrine and dopamine, help with communication between brain cells. It might take some time to find the right medication at the right dose for you.

These are some of the most commonly prescribed medications for depression:
Selective serotonin reuptake inhibitors (SSRIs). Doctors commonly start by prescribing this class of medication. SSRIs generally cause fewer side effects than other types of antidepressants. Common SSRIs include:
Serotonin and norepinephrine reuptake inhibitors (SNRIs). In addition to depression, SNRIs are also often used to treat anxiety and chronic pain (especially nerve pain). Examples of SNRIs include:
Atypical antidepressants. These medications are known as atypical because they don’t fit the other antidepressant categories. You might take them if other antidepressants haven’t worked well for you or have caused serious side effects. Atypical antidepressants include:
Tricyclic antidepressants. These are the oldest of the antidepressants. Because they tend to cause more side effects, they aren’t used as often anymore. They’re usually prescribed if other antidepressant medications aren’t working for you. They include:
Monoamine oxidase inhibitors (MAOIs). MAOIs — such as tranylcypromine (Parnate®) and phenelzine (Nardil®) — may be prescribed if other medications don’t work well for you. MAOIs have serious side effects and require a strict diet due to dangerous and sometimes deadly interactions with foods such as aged cheeses, wine and pickles. A newer MAOI, selegiline (Emsam®), is worn as a patch on the skin and has fewer side effects.
Other medications. To strengthen an antidepressant’s effects, your doctor may prescribe other medications. They might combine two antidepressants or add mood stabilizers or antipsychotics. Antianxiety and stimulant medications also may temporarily be added.
Some experts are looking at microdosing (using tiny, controlled amounts) with psychedelics such as psilocybin for treatment-resistant depression. There’s also a Food and Drug Administration (FDA)–approved nasal spray called esketamine (Spravato®), which is based on an anesthetic called ketamine. This medication, when used with an antidepressant that’s taken by mouth, can be highly effective for people who’ve tried other medications without success, according to the FDA.
And early research suggests that CBD (cannabidiol, a component of marijuana plants that doesn’t cause a high) may help. But talk to your provider before trying anything along these lines, since sometimes these substances may not be advised with a medication you’re already taking.
The benefits of an antidepressant can take some time to kick in, so you might have to wait 4 to 6 weeks to see positive effects after you start taking the medication. During that time, be sure to keep up with your therapy appointments and any other lifestyle changes your provider recommends.
Depression can make it difficult to take care of yourself. You might not want to eat nutritious foods, go to the gym, be outside in the fresh air and sunshine, or spend time with people. But these are all important parts of getting and staying better. Try to do a little something every day and eventually you’ll find that it’s easier to get motivated.
Like many medications, antidepressants can have side effects, but not everyone experiences them, and some folks only experience mild ones. The most common side effects of antidepressants are:
If you think you might be experiencing a side effect, talk to your doctor or pharmacist.
And most important: Don’t just stop taking your antidepressants on your own. That can cause withdrawal symptoms such as dizziness and nausea, or more dangerous symptoms such as the return of your depression symptoms. Instead, your doctor will work with you to gradually decrease your dose safely.
If the most common depression treatments aren’t working for you, don’t despair: There are other options.
Electroconvulsive therapy (ECT). This procedure applies controlled electric currents to the brain while you are sedated. It causes a controlled seizure that can affect neurons and chemicals in the brain.
While this sounds scary, today’s ECT is much safer than the “electric shock therapy” that was done in the 1960s and 1970s. There are possible side effects, including mild memory lapses, but they are usually temporary.
The procedure is most often used on people with severe depression and/or psychosis who don’t benefit from medication, and it can be quite effective. In fact, about 80% of people with severe depression will have a significant improvement in symptoms after ECT, according to the American Psychiatric Association. ECT is also sometimes used to treat bipolar disorder.
Transcranial magnetic stimulation (TMS). This procedure stimulates nerve cells in the brain with electromagnetic fields. A large electromagnetic coil is placed on the patient’s forehead, and short pulses are then directed into an area of the brain thought to control moods.
Because it’s noninvasive, it’s generally safe. However, TMS should not be used on people who have depression with psychosis, bipolar disorder or suicidal thoughts. (You also can’t be treated with TMS if you have a pacemaker or if you have metal objects in your head.)
In cases of severe depression, or if someone is a danger to themselves or others, hospitalization may be needed. If you have thoughts of suicide, get medical help right away. Call 911 if you have an emergency.
You can also call the Suicide Prevention Lifeline at 1-800-273-8255, or go to suicidepreventionlifeline.org/chat for a live chat. Your therapist can also help you create a safety plan if you’re experiencing thoughts of death or suicide.
Depression is a very treatable disease. In fact, it’s one of the most treatable mental illnesses because of how much research has been done on it.
Because hopelessness is one of the hallmark symptoms of depression, it can be challenging to believe that you can improve and to take the first step of getting help. But know this: At least 80% of people with depression respond very well to treatment, according to the National Institutes of Mental Health. And with professional help, almost everyone with depression experiences some relief from their symptoms.
When your depression symptoms are improving, it shouldn’t be subtle. You’ll notice yourself smiling and laughing more and generally enjoying life again. You might still experience some symptoms, but they won’t make it as hard to function and to enjoy your life again.
And once your mood improves, you should also see improvements to your sleep patterns and energy levels. It will be easier to get up and move in the morning or finish a task at work. You might also feel less overwhelmed.
It’s not uncommon for people to experience depression more than once during their lifetime. A loss or an upsetting event might make you tearful for several days or a week, or you might find it hard to sleep. But getting treatment early, and using the coping strategies and behavioral changes you’ve learned in therapy, can help reduce those relapses or help you rebound more quickly.

We can help you find a licensed therapist and even supply medication if you need it — no insurance required.
Drew Ramsey, MD
Assistant clinical professor of psychiatry at Columbia University College of Physicians and Surgeons
New York City
Peggy Scallon, MD
Psychiatrist and medical director of Focus Depression Recovery Adolescent Residential Care at Rogers Behavioral Health
Oconomowoc, Wisconsin
Major depressive disorder: Canadian Journal of Psychiatry (2014). “Cognitive Dysfunction in Major Depressive Disorder: Effects on Psychosocial Functioning and Implications for Treatment”
Gender facts on major depression: National Institute of Mental Health. Major Depression and Men and Depression. Symptoms of depression and demographic statistics: Centers for Disease Control and Prevention. Symptoms of Depression Among Adults
Facts on depression: Centers for Disease Control and Prevention. Mental Health Conditions: Depression and Anxiety. National Alliance on Mental Health. Depression.
Postpartum depression: National Institute of Mental Health: Perinatal Depression; and Office on Women’s Health. Postpartum Depression.
Statistics, symptoms, progression of depression in pregnant women: Cleveland Clinic Journal of Medicine. 2020. Perinatal Depression: A Review.
Premenstrual dysphoric disorder: Johns Hopkins Medicine. Premenstrual Dysphoric Disorder; US National Library of Medicine. Premenstrual Syndrome
Depression and inheritability; therapy for depression: American Psychiatric Association. What is Depression?
Diagnosing depression: U.S. National Library of Medicine. Appendix 12: “The classification of depression and depression rating scales/questionnaires”
Microdosing: Therapeutic Advances in Psychopharmacology 2020. “The therapeutic potential of microdosing psychedelics in depression”
Spravato: US Food and Drug Administration. 2019 “FDA Approves New Nasal Spray”
Esketamine: Johns Hopkins Medicine. Esketamine For Treatment Resistant Depression.
CBD: Harvard Medical School. Cannabidiol (CBD): What We Do and Don’t Know about
ECT: American Psychiatric Association. What Is Electroconvulsive Therapy?
Brain stimulation techniques: National Alliance on Mental Illness. ECT, TMS and Other Brain Stimulation Therapies
Improvement with treatment: National Institute of Health Collaborative Program. The time course of nonchronic major depressive disorder.